- A new scientific statement from the American Heart Association (AHA) reveals a strong link between cardiovascular diseases — such as heart failure, atrial fibrillation and coronary heart disease — and an increased risk of cognitive impairment and dementia.
- The research explains how heart health directly impacts brain function, with conditions like high blood pressure and type 2 diabetes therefore contributing to cognitive decline.
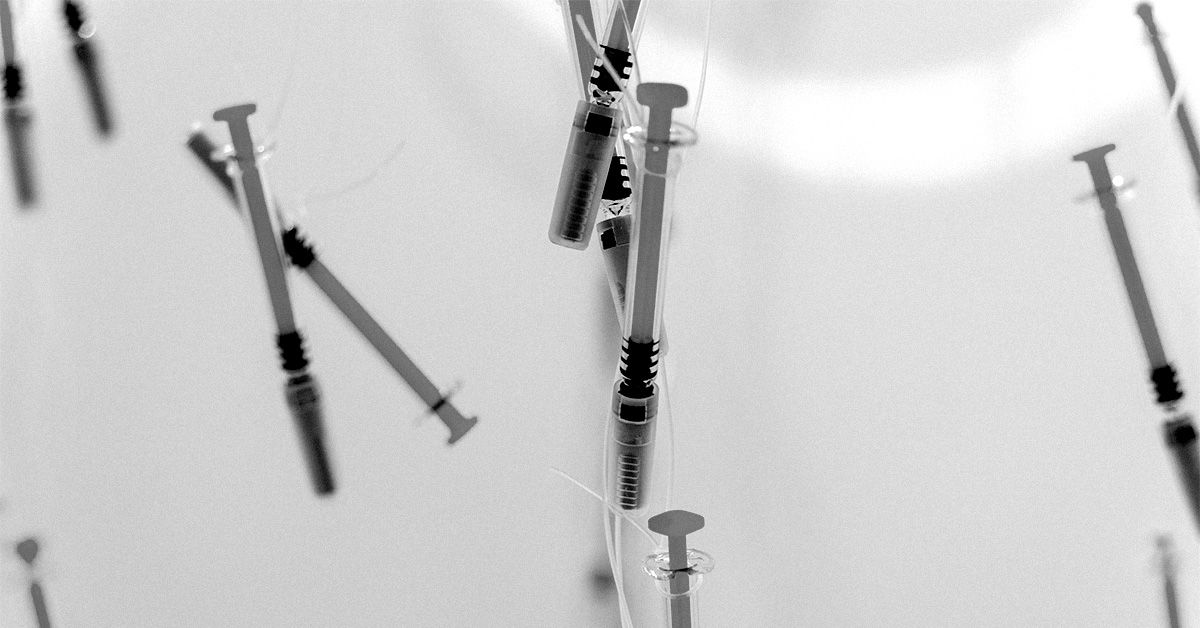
- In another new study, researchers suggest that the blood thinner heparin may delay the onset of Alzheimer’s disease by interfering with harmful protein interactions in the brain; however, more research is needed.
The authors point out that stroke and cognitive decline, two significant factors in brain health, are chronic and disabling conditions that greatly impact individuals and society.
Maintaining heart health from a young age is essential to prevent cardiovascular diseases, protect brain function and lower the risk of cognitive decline later in life.
While dementia is often seen as an untreatable and progressive condition, evidence suggests that leading a healthy lifestyle and addressing vascular risk factors early on may help preserve cognitive function.
According to the studies highlighted in the AHA report, heart failure affects around 50% of people with cognitive issues, such as memory and language difficulties.
AFib, the most common heart rhythm disorder, is linked to a 39% increased risk of cognitive impairment, while coronary heart disease increases the risk of dementia by 27%, with up to 50% of heart attack survivors experiencing cognitive decline.
Previous research showed that people with AFib who were treated with direct oral anticoagulants (DOACs) had a 12% lower risk of developing dementia compared to those treated with the traditional blood thinner warfarin.
Now, in a new study whose results appeared in Molecular Psychiatry, researchers found that people undergoing heparin treatment developed Alzheimer’s symptoms up to 2 years later than the typical timeframe, also indicating a potential protective benefit of this common anticoagulant.
Previous research demonstrated that the risk of developing Alzheimer’s may be linked to a protein called Apolipoprotein E (ApoE), which interacts with cell surface molecules known as heparan sulfate proteoglycans (HSPGs).
The ApoE4 genetic variant is associated with the highest risk, while a rare form, ApoE Christchurch, binds weakly to HSPGs and appears to reduce the risk of Alzheimer’s in genetically predisposed individuals.
HSPGs also contribute to the buildup of tau protein, another key factor in Alzheimer’s brain damage.
Proteins that bind to HSPGs may accumulate in the brain long before symptoms appear and a gene involved in heparan sulfate production has been identified as an Alzheimer’s risk factor.
Heparin, a form of heparan sulfate used since the 1930s to prevent blood clots, does not enter the brain, but researchers speculate it could delay Alzheimer’s by disrupting ApoE-HSPG interactions.
In this new study, researchers analyzed medical records from two large health systems, Mount Sinai Health System (MSHS) and Columbia University Medical Center (CUMC).
Using a retrospective, longitudinal design, they compared patients who had received heparin to those who had not.
In the MSHS cohort, 24.7% of the 15,183 patients had received heparin, while 51.5% of the 6,207 CUMC patients had undergone heparin treatment.
While all the study participants eventually received an Alzheimer’s diagnosis, on average, patients in either cohort who received heparin got an Alzheimer’s diagnosis about 1 year later than those who did not.
The study’s first author, Benjamin Readhead, PhD, a research associate professor at the ASU-Banner Neurodegenerative Disease Research Center, explained the key findings to Medical News Today.
“Some of our co-authors had previously shown that a rare genetic mutation in the APOE gene is actually very protective against Alzheimer’s disease, and that this had something to do with disrupting how that version of the APOE protein binds to heparin-like molecules within the body,” Readhead told us.
“We wondered whether there might be a way of studying this by looking at the anticoagulant medicine heparin, and whether its usage seems to offer any protection against Alzheimer’s disease. When we looked at electronic health records (EHR) from two large health systems, we found that in both EHR, heparin therapy was associated with a significant delay of about 1 year in the clinical diagnosis of [Alzheimer’s disease] dementia.”
– Benjamin Readhead, PhD
Eric M. Reiman, MD, the study’s senior author, told MNT that “while the findings have no implications for the use of current heparin formulations in the treatment and prevention of Alzheimer’s disease, the study could help inform the development of new disease-modifying treatments for Alzheimer’s disease, including in carriers of the APOE4 gene, the major genetic risk factor for [Alzheimer’s].”
Reiman pointed out that the study looked at a specific group of people who have a higher risk of developing Alzheimer’s due to their genetics.
The findings, that a rare version of APOE might help protect against the symptoms of Alzheimer’s, led the researchers to think that if they could block APOE from sticking to HSPG, it might be possible to create a treatment or even prevent Alzheimer’s.
Clifford Segil, DO, a neurologist at Providence Saint John’s Health Center in Santa Monica, CA, not involved in this research, said that although “it is challenging to claim a ‘blood-thinning’ medication could affect [Alzheimer’s disease development], […] when it would be more likely this family of medications would protect against a certain type of dementia from recurrent strokes caused [by] multi-infarct dementia or vascular dementia.”
He cautioned that: “After reviewing this paper, I would think heparin use should not be assumed to prevent Alzheimer’s [disease], and I would like a follow-up study to determine if, in hospital, heparin use can cause a decrease in stroke dementias or vascular dementia, which may also be called multi-infarct dementia.”
Reiman added that this study “illustrates the opportunity to use large EHR data sets to evaluate the effects of different drugs in the treatment and prevention of [Alzheimer’s disease].”
“This information could be used to support further assessments of potentially repurposed drugs in the treatment and prevention of [Alzheimer’s disease] or, as illustrated in this particular case, provide new information about the biological changes that could be targeted in the development of new drug therapies.”
– Eric M. Reiman, MD
The researchers also considered whether heparin could help protect brain health, more generically.
However, because most forms of heparin do not easily reach the brain and are only used for short periods, it was uncertain if it would be effective as a brain-health-protective drug.
While more research is needed, the findings from analysing large sets of patient data suggest that it may be possible to develop drugs targeting this process.
These potential new treatments could be tested in experimental models in the future.
Read the full article here